Types Of Psoriatic Arthritis
Psoriatic arthritis is a chronic inflammatory disease that affects millions of people worldwide. It occurs when the immune system attacks healthy tissues and cells in the body, leading to joint pain, swelling, and stiffness. Psoriatic arthritis is often associated with psoriasis, a skin condition that causes red, scaly patches on the skin. However, not everyone with psoriasis develops psoriatic arthritis.
There are several types of psoriatic arthritis, each with its own set of symptoms and characteristics. These include asymmetrical arthritis, symmetrical polyarthritis, distal interphalangeal predominant (DIP) arthritis, spondylitis, and arthritis mutilans. Asymmetrical arthritis is the most common type and affects one or more joints on one side of the body. Symmetrical polyarthritis affects multiple joints on both sides of the body, while DIP arthritis primarily affects the joints closest to the nails. Spondylitis affects the spine, causing pain and stiffness in the neck and lower back. Arthritis mutilans is a rare but severe form of psoriatic arthritis that can cause deformities in the hands and feet.
Key Takeaways
- Psoriatic arthritis is a chronic inflammatory disease that affects the joints and skin.
- There are several types of psoriatic arthritis, each with its own set of symptoms and characteristics.
- Treatment options for psoriatic arthritis include medication, physical therapy, and lifestyle changes.
Understanding Psoriatic Arthritis
Psoriatic arthritis (PsA) is a chronic inflammatory disease that affects the joints and skin. It is a type of arthritis that occurs in people who have psoriasis, a skin condition that causes red, scaly patches on the skin. PsA can cause joint pain, stiffness, and swelling, as well as skin changes such as nail pitting and scaly patches.
Causes and Risk Factors
The exact cause of PsA is not known, but it is believed to be related to an overactive immune system. In people with PsA, the immune system attacks healthy tissues in the joints and skin, causing inflammation and damage. Genetics may also play a role in the development of PsA, as it tends to run in families.
Other risk factors for PsA include having psoriasis, a history of joint injuries or infections, and being overweight or obese. Smoking and stress may also increase the risk of developing PsA.
Common Symptoms
PsA can cause a wide range of symptoms, which can vary from person to person. The most common symptoms of PsA include joint pain, stiffness, and swelling, especially in the fingers, toes, and lower back. Other symptoms may include fatigue, nail changes, and skin patches that are red, scaly, and itchy.
Diagnosing Psoriatic Arthritis
Diagnosing PsA can be challenging, as it can mimic other types of arthritis and may not always be associated with psoriasis. A doctor will typically perform a physical exam, review the patient’s medical history, and order imaging tests such as X-rays, MRI, or ultrasound to help diagnose PsA.
Blood tests may also be ordered to check for inflammation and to rule out other conditions. A skin biopsy may be performed if psoriasis is suspected but not obvious.
In conclusion, Psoriatic arthritis is a chronic inflammatory disease that affects the joints and skin. It is caused by an overactive immune system that attacks healthy tissues in the joints and skin. PsA can cause joint pain, stiffness, and swelling, as well as skin changes such as nail pitting and scaly patches. Diagnosing PsA can be challenging, but with the right tests and evaluations, it can be accurately diagnosed.
Types of Psoriatic Arthritis
Psoriatic arthritis is a type of arthritis that affects some individuals who have psoriasis. There are five main types of psoriatic arthritis, categorized by the type of joint impacted. People can have one type initially only to develop another type later on.
Symmetric Psoriatic Arthritis
Symmetric psoriatic arthritis is the most common type of psoriatic arthritis, affecting approximately 50% of individuals with psoriatic arthritis. It is similar to rheumatoid arthritis in that it affects the same joints on both sides of the body. The joints that are usually affected include the fingers, toes, wrists, and knees.
Asymmetric Psoriatic Arthritis
Asymmetric psoriatic arthritis is another common type of psoriatic arthritis, affecting approximately 35% of individuals with psoriatic arthritis. This type of psoriatic arthritis affects joints on one side of the body only. It can affect any joint, but it most commonly affects the fingers and toes.
Distal Interphalangeal Predominant (DIP)
Distal interphalangeal predominant (DIP) psoriatic arthritis is a rare type of psoriatic arthritis that affects the distal joints of the fingers and toes. This type of psoriatic arthritis is often confused with osteoarthritis or gout.
Spondylitis
Spondylitis is a type of psoriatic arthritis that affects the spine and neck. It is common in people living with psoriatic arthritis and can occur with other forms of psoriatic arthritis at the same time. Spondylitis can cause pain and stiffness in the neck and lower back.
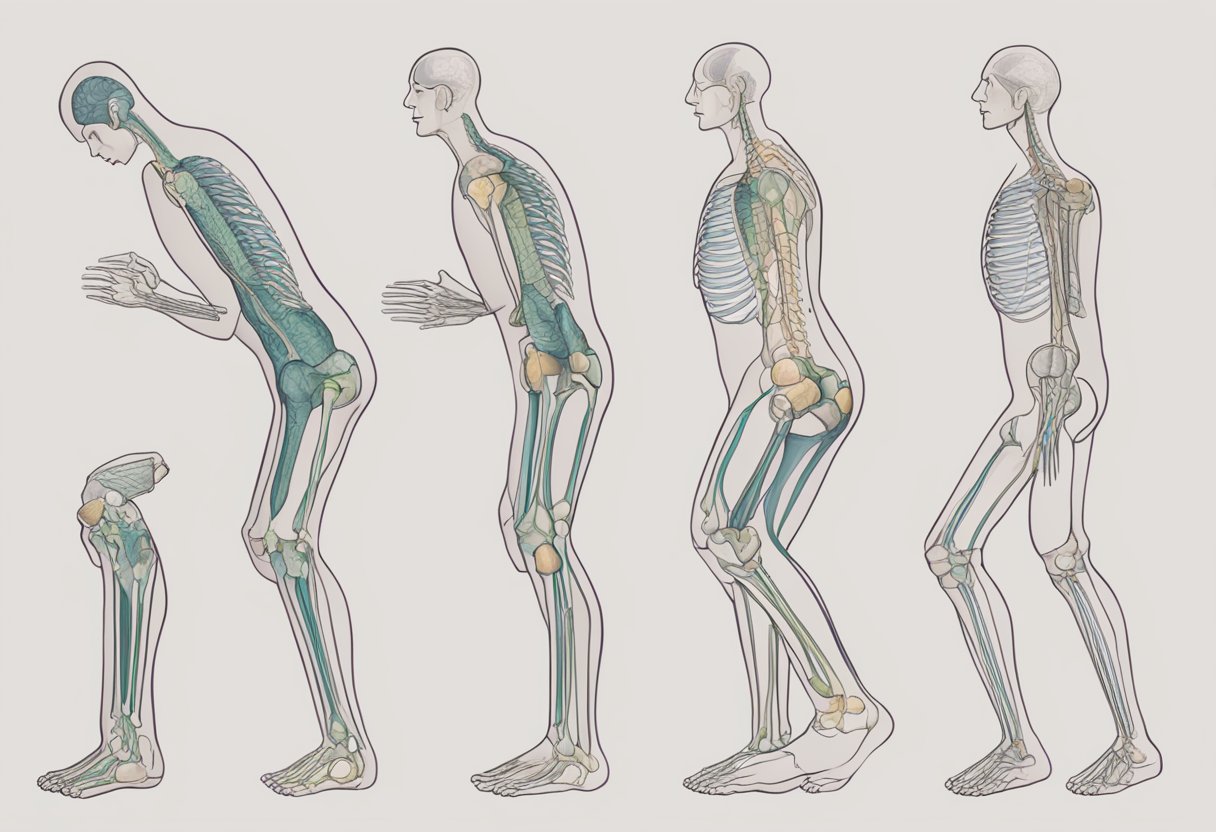
Arthritis Mutilans
Arthritis mutilans is a rare and severe form of psoriatic arthritis that can cause joint damage and deformity. It usually affects the small joints in the hands and feet. Arthritis mutilans can cause fingers and toes to become shortened and misshapen, giving them a “telescoping” appearance.
In summary, psoriatic arthritis is a complex disease with various types, each affecting different joints in the body. Understanding the different types of psoriatic arthritis is crucial in the diagnosis and treatment of this condition.
Treatment Options
Psoriatic arthritis is a chronic disease that requires long-term management to control symptoms and prevent joint damage. Treatment options for psoriatic arthritis include medications, surgical interventions, and lifestyle and home remedies.
Medications
There are several types of medications used to treat psoriatic arthritis, including nonsteroidal anti-inflammatory drugs (NSAIDs), disease-modifying antirheumatic drugs (DMARDs), biologics, and steroids. NSAIDs can help reduce pain and inflammation, while DMARDs can slow down the progression of joint damage. Biologics target specific parts of the immune system to reduce inflammation, and steroids can be used to quickly reduce inflammation and pain.
Surgical Interventions
Surgery is generally not a common treatment option for psoriatic arthritis, but it may be necessary in some cases. Joint replacement surgery may be recommended if joint damage is severe and other treatments have not been effective.
Lifestyle and Home Remedies
In addition to medications and surgical interventions, lifestyle changes and home remedies can also help manage symptoms of psoriatic arthritis. Exercise, such as yoga and stretching, can help improve flexibility and reduce pain. Meditation and other relaxation techniques can also help reduce stress and improve overall well-being. Making dietary changes, such as avoiding inflammatory foods, can also help manage symptoms.
Overall, psoriatic arthritis is a complex condition that requires a multifaceted approach to treatment. With the right combination of medications, surgical interventions, and lifestyle changes, people with psoriatic arthritis can manage their symptoms and improve their quality of life.
Managing Symptoms and Complications
Psoriatic arthritis can cause a wide range of symptoms that can impact a person’s daily life. However, there are ways to manage these symptoms and reduce their severity.
Pain Management
Pain is one of the most common symptoms of psoriatic arthritis. Over-the-counter pain relievers such as acetaminophen or nonsteroidal anti-inflammatory drugs (NSAIDs) can help manage mild to moderate pain. For more severe pain, prescription pain medications may be necessary.
In addition to medication, other pain management techniques such as heat or ice therapy, massage, and acupuncture may also be helpful in reducing pain.
Mobility and Physical Therapy
Stiffness and swelling in the joints can make it difficult to move and perform daily activities. Physical therapy can help improve mobility and reduce stiffness. A physical therapist can create a personalized exercise plan to improve range of motion, flexibility, and strength.
Occupational therapy can also be helpful in teaching individuals how to perform daily tasks with less pain and strain on the joints.
Mental and Emotional Health
Living with psoriatic arthritis can be challenging and can impact a person’s mental and emotional health. Depression and anxiety are common in individuals with chronic pain conditions.
It is important to seek support from friends, family, or a mental health professional. Support groups can also be helpful in connecting with others who are going through similar experiences.
Overall, managing symptoms and complications of psoriatic arthritis requires a multidisciplinary approach that includes medication, physical therapy, and emotional support. By working with healthcare providers and making lifestyle changes, individuals with psoriatic arthritis can improve their quality of life.
Living with Psoriatic Arthritis
Psoriatic arthritis can be a challenging condition to live with, but there are ways to manage symptoms and maintain a good quality of life. This section will explore some strategies for coping with psoriatic arthritis on a daily basis, finding support, and looking towards the future.
Daily Life and Activities
Living with psoriatic arthritis may require some adjustments to daily life and activities. For example, individuals with psoriatic arthritis may find that they need to take breaks more frequently or modify their activities to avoid joint pain. It may also be helpful to incorporate regular exercise into daily routines, such as walking or swimming, to help improve joint flexibility and reduce stiffness.
Support and Coping Strategies
Finding support and coping strategies can be an important part of managing psoriatic arthritis. Support groups, counseling, and other resources can provide individuals with the emotional support and practical advice they need to cope with the challenges of living with psoriatic arthritis. It may also be helpful to develop strategies for managing stress, such as mindfulness or relaxation techniques.
Long-Term Outlook
While psoriatic arthritis can be a chronic condition, there are many treatment options available that can help manage symptoms and slow down the progression of the disease. With the right treatment and lifestyle changes, individuals with psoriatic arthritis can lead fulfilling and active lives. It is important to work closely with a healthcare provider to develop a long-term treatment plan that is tailored to individual needs and goals.
In summary, living with psoriatic arthritis can be challenging, but there are many strategies that can help manage symptoms and improve quality of life. Incorporating regular exercise, finding support, and working closely with a healthcare provider can all be important steps towards managing psoriatic arthritis and looking towards the future.






